Elective recovery loses more momentum
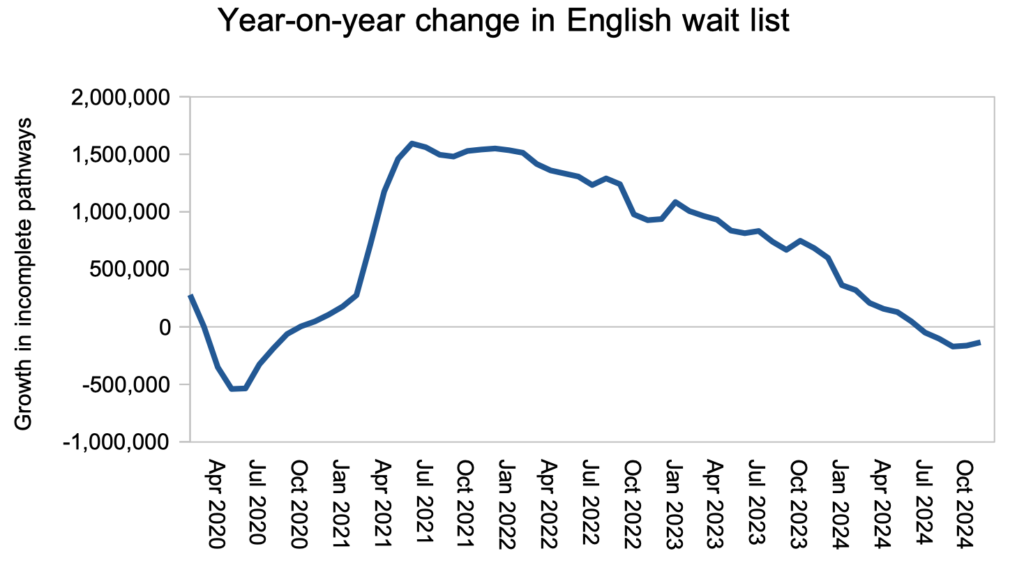
The pace of England’s elective recovery slowed again in November. On the reported figures, the waiting list reduced year-on-year by just 134,000 patient pathways to the end of November, down from October’s 162,000, and much lower than September’s peak of 195,000. The NHS needs to reach a reduction rate of roughly one million per year to restore the 18 week referral-to-treatment (RTT) standard by March 2029.
The NHS will also be scratching their heads about NHS England’s new style of waiting time target. Instead of bringing down long RTT waiting times, hospital trusts must now increase the percentage of the waiting list that is within 18 weeks.
A good response would harness the ongoing expansion in outpatient and diagnostic capacity, to reduce the waiting time for diagnosis and decision to 18 weeks. That would sharply improve the waiting time experience for most patients, avoid the clinical risks of long-waiting undiagnosed patients, and curb the cost of administering huge numbers of waiting list patients, all at a relatively low cost per case, while maximising the contribution of those waiting list stages towards the new percentage target.
The consequence of reducing waiting times for outpatients and diagnostics will be an increase in patients added to the next stage of the waiting list, for inpatient and daycase treatment. It will be important not to lose control of this waiting list for admission, and the NHS will need to plan carefully to avoid building up an insuperable problem for later years.
In the following discussion, all figures come from NHS England. You can look up your trust and its prospects for achieving the waiting time targets here.
The numbers
The year-on-year reduction in waiting list size faltered for the second month in a row, instead of continuing towards the one million per year level required to restore 18 weeks by 2029 as the government has pledged. (About 50,000 of the reduction this financial year is an artefact of counting changes, and there are very large numbers of patients missing from the numbers because most trusts do not follow the rule that overdue follow-up outpatients should start waiting time clocks.)
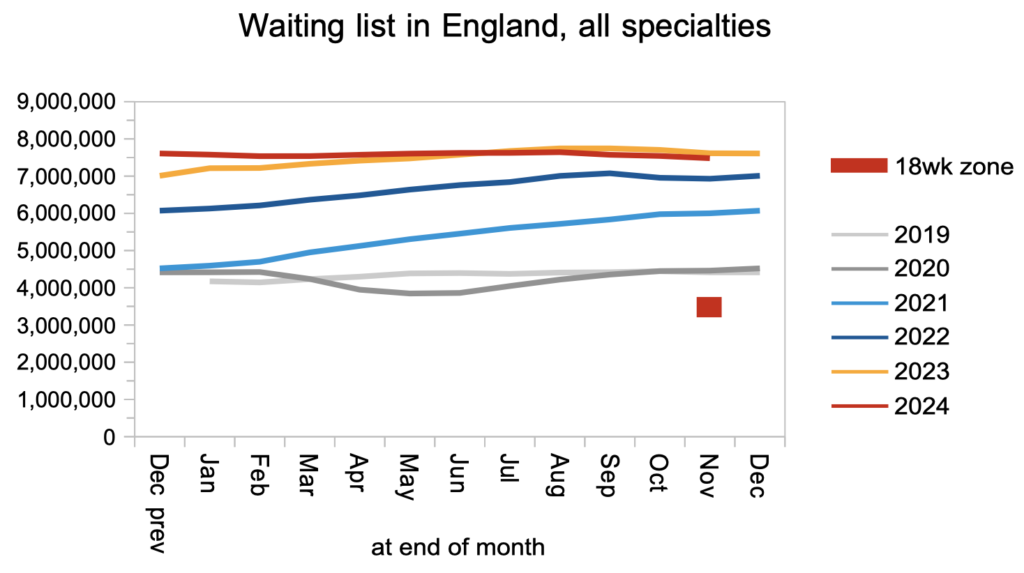
The RTT waiting list size was 7.5 million patient pathways at the end of November. Some 6.3 million of them are waiting for a diagnosis and decision, so outpatients and diagnostics is where the sheer numbers are. The NHS is adding significant capacity to do more of this relatively low cost activity, and a good thing too, because there is inherent risk in keeping undiagnosed patients waiting long periods of time.
At the end of November, the typical wait for diagnosis and decision was 40.4 weeks, which is far too long for the estimated 27,314 of those patients whose eventual diagnosis will unexpectedly be cancer.

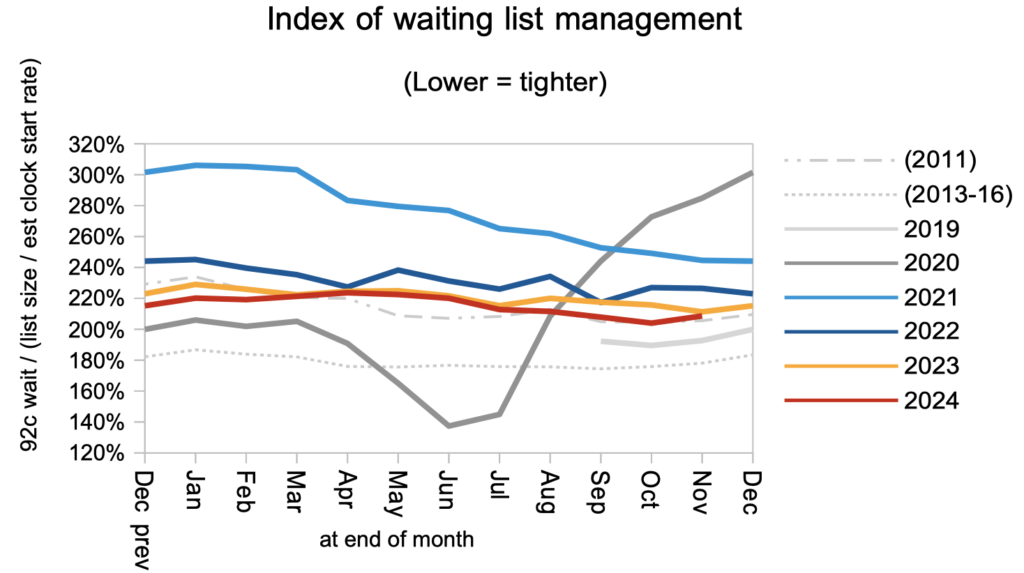
Waiting times are a function of both the size and shape of the waiting list, and the shape remained at 2011 levels in November. It is likely to improve naturally in the comings years as the 18 week standard is restored, but the recent decision to target the percentage within 18 weeks instead of long waits might result in this metric deteriorating over the coming year.
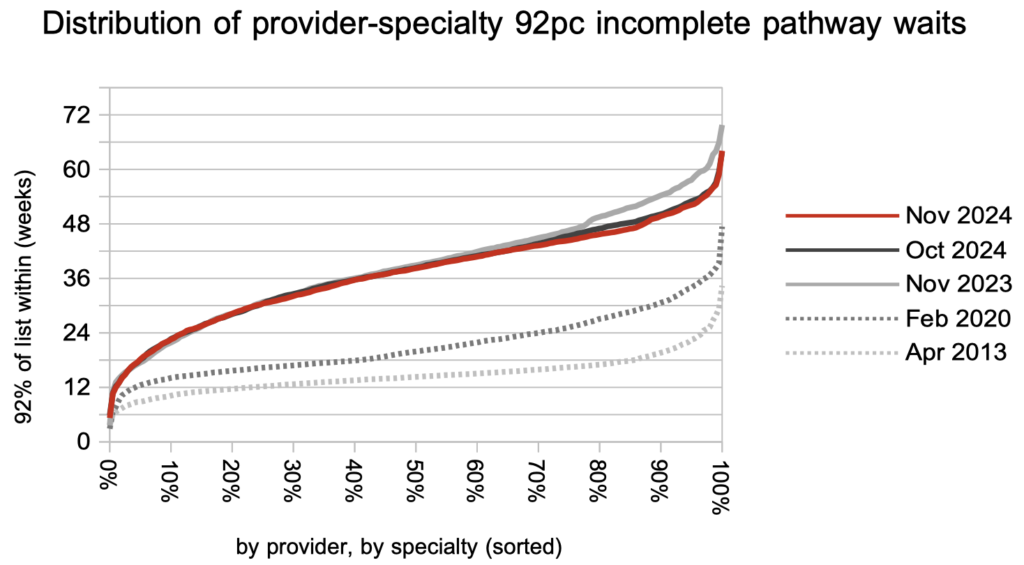
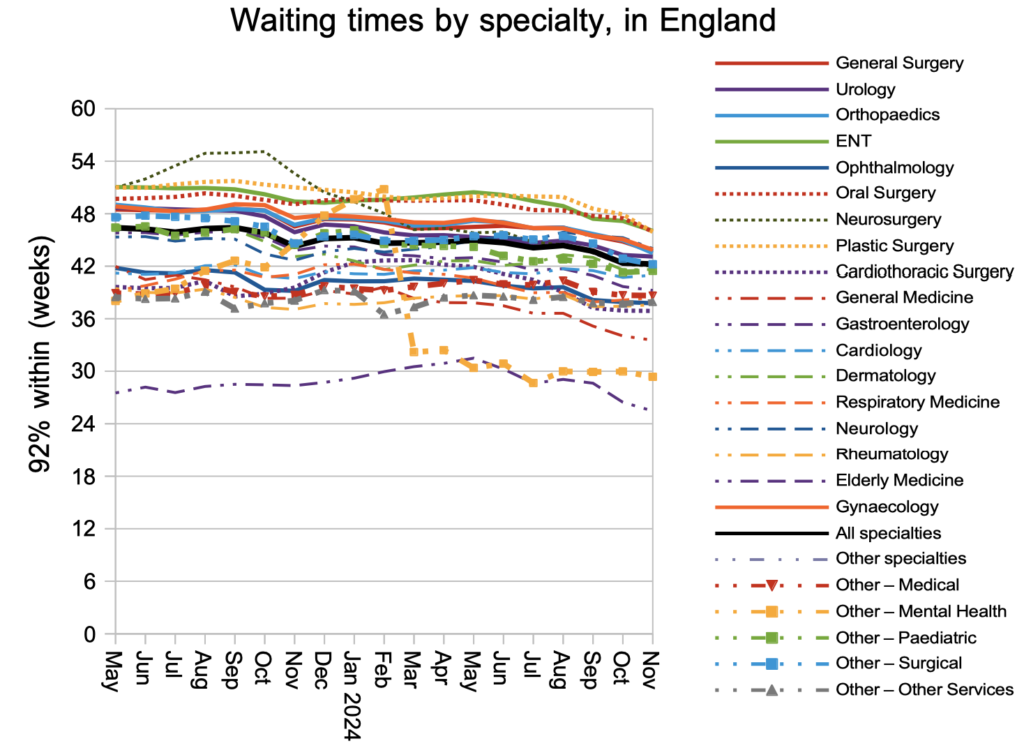
Waiting times continued to edge downwards at the longest-waiting end of the distribution, in response to the current targets to eliminate ultra long waits. If there are no supplementary controls on long waiters next financial year then this could slip back, building up problems for the later years of elective recovery.
It is good to see improvements in waiting times in the longest-waiting specialties.
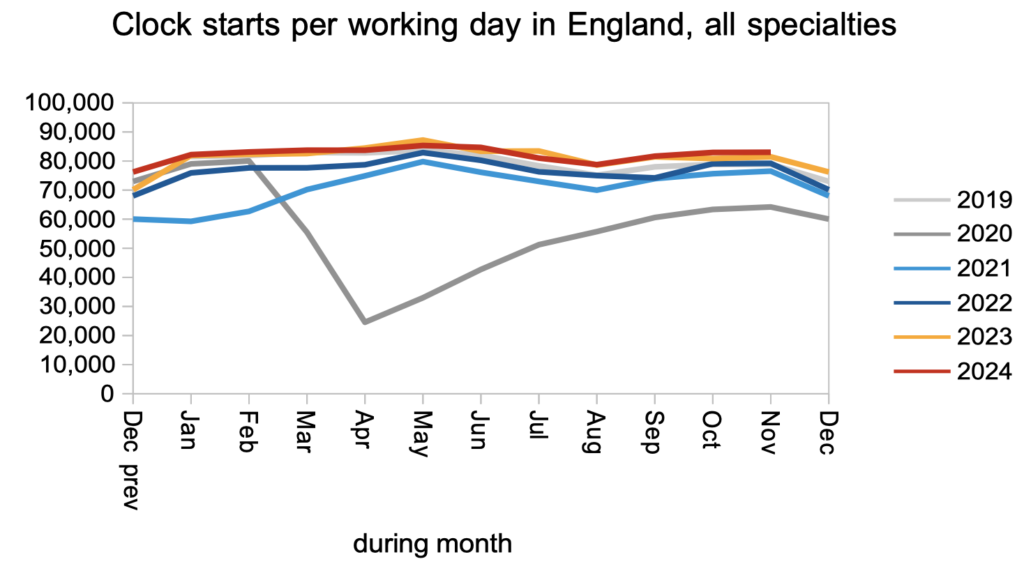
Finally, a quick look at demand versus activity. Demand remained similar to last year, according to the numbers of patients starting new waiting time ‘clocks’.
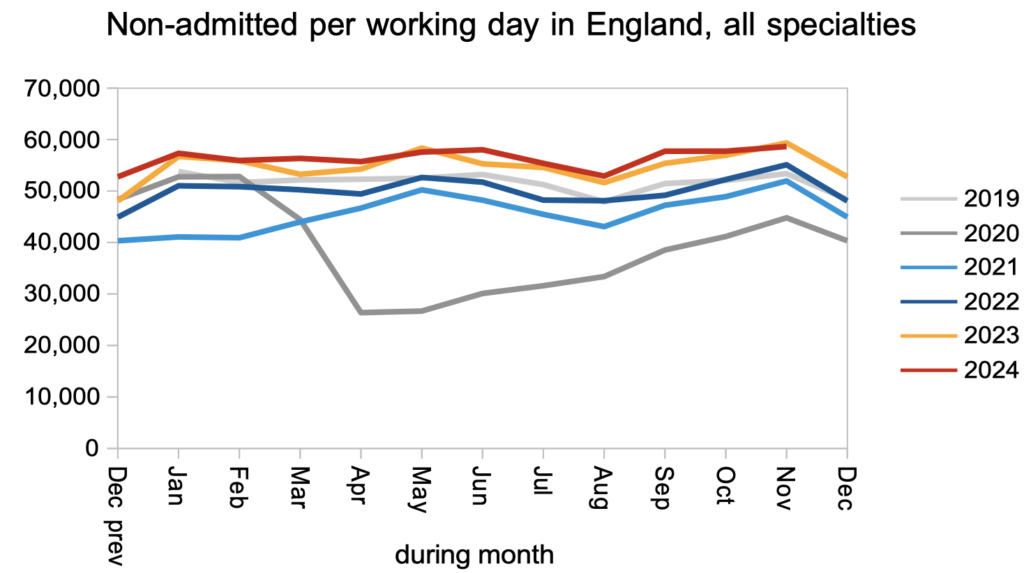
Patients were discharged from outpatient clinics and diagnostics at similar rates to last year. This rate will need to increase significantly over the coming months to get the elective recovery underway. When that happens, more patients will be found who need admitting for inpatient or daycase treatment.
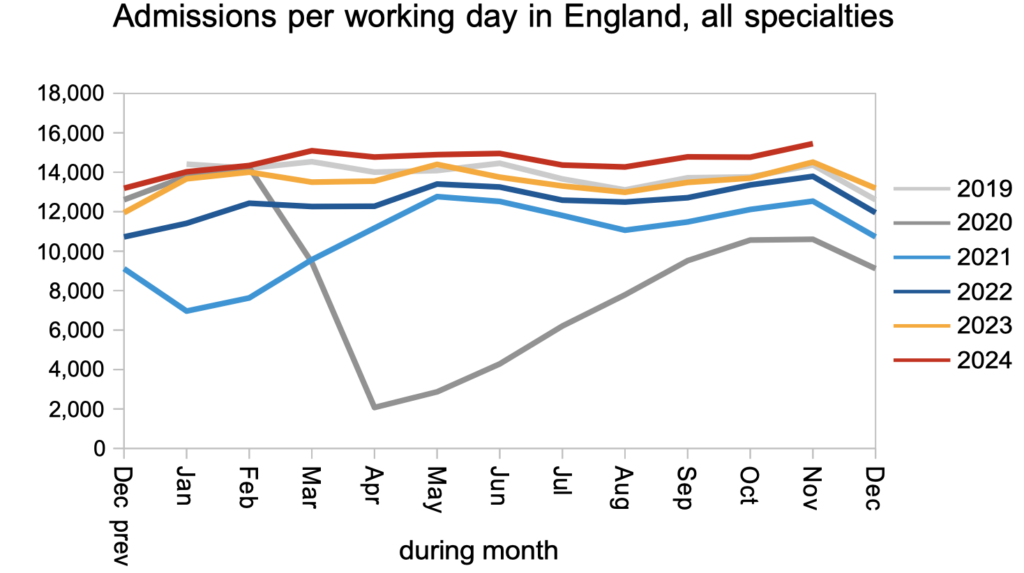
Patients were admitted for inpatient and daycase treatments significantly faster than last year, which will need to continue to catch the extra demand caused by clearing the outpatient and diagnostics backlog.
Referral-to-treatment data up to the end of December is due out at 9:30am on Thursday 13th February.
