
18-weeks targets push pressured Trusts into perverse patient scheduling
10/06/2014by Rob Findlay
33 per cent of pressured hospital specialties booked patients out of order to meet government targets last financial year, and 58 per cent of English Trusts did so in at least one specialty. This shows that despite the introduction of the incomplete pathways target in April 2013, the perverse admitted and non-admitted targets still retain their power to distort patient management, a power that was increased this April when higher penalties were attached to the admitted target.
Elective waiting lists should be managed around the needs of patients: safe, fair and short. Everybody agrees on that, at least in principle.
But things aren’t always that simple in practice, because in England the admitted patient target means stiff penalties for hospitals who treat too many long-waiting patients. I’ve discussed these perverse incentives many times before, but here I want to look at their effect in real life. To what extent do perverse incentives translate into perverse actions? Or do hospitals manage to negotiate around them and do the right thing for their patients?
Perversity in practice
We know that sometimes hospitals “manage to the target” instead of managing to patients’ needs. Here is an example. I won’t tell you where it is, because there are so many examples and I could have picked any of them.
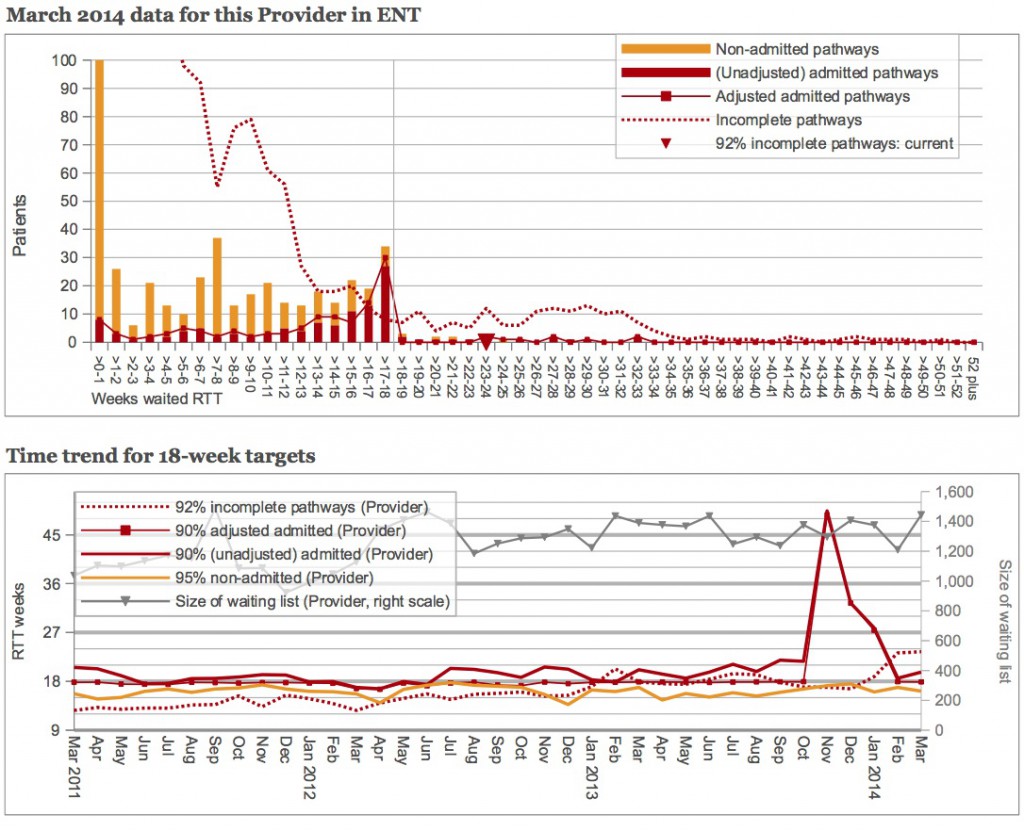
The top chart shows this service’s most recent 18-weeks data. The dotted red line shows the waiting list at month-end (incomplete pathways, in the jargon) and as you can see there are plenty of long-waiting patients stretching all the way out beyond 30 weeks with some waiting nearly a year. What have they been doing about them? Not a lot. The red and orange columns show which patients were treated during the month: plenty of short-waiters were treated, but hardly any long-waiters.
The bottom chart shows what has been happening over time. The thin red blobby line shows performance against 90 per cent adjusted admitted waiting times. It clings tightly to the underside of the 18-week target throughout the time series.
Actually, not quite throughout. From November 2013 to January 2014 this service made a valiant effort to admit its long-waiting patients, even though this meant breaching this particular target. That held down waiting times for a while, but then they scurried quickly back inside the target which let waiting times blow out again.
So this is a pretty clear picture of a service that managed to a perverse target, instead of doing the right thing and treating the longest-waiting patients. Whose fault is it? Perhaps the hospital should have ignored the target and put the needs of patients first? That’s easy to say when you don’t have hefty contractual penalties, Monitor, the CQC, and the local press breathing down your neck. The target-enforcers need to take a good hard look at their actions too.
How widespread?
Now let’s see how common this is. We’ll look only at surgical specialties in English NHS Trusts, excluding any with small volumes or incomplete data: that’s 794 services in all. And we’ll look only at their monthly data since April 2013, which is when penalties began for breaching the incomplete pathways target.
At the end of any month, on average 191 (24 per cent) of those 794 services breached the “incomplete pathways” target (that 92 per cent of the waiting list must be within 18 weeks).
A higher number, 244 (31 per cent), breached the “adjusted admitted” target (that 90 per cent of admitted patients, i.e. inpatients and daycases, must have waited less than 18 weeks, adjusting for any clock pauses). That higher number makes sense, because this target is tougher than the incomplete pathways target.
Only 142 services (18 per cent) breached the “non-admitted” target (that 95 per cent of non-admitted patients, i.e. outpatients, must have waited less than 18 weeks). Again that makes sense because in surgical specialties most outpatient discharges happen early in the pathway.
Now, amongst all that, how can we detect perverse patient scheduling?
We could look for it simply by searching for services where (in the same month) the incomplete pathways target is being breached, but not the admitted patients target. There are two problems with that. Firstly, the incomplete pathways measurement is taken at the end of the month, whereas it is the start of month position that shows there are long-waiters needing treatment. Secondly, it leaves open the possibility that the longest-waiting patients could be waiting for treatment in clinic.
So the test we will apply is this. We will survey services (at Trust-specialty level) where the incomplete pathways target was breached at the start of the month (showing that there were initially lots of long-waiters on the waiting list). We will only score that service as managing perversely to the target if: neither the adjusted admitted nor the non-admitted targets were breached during the month (showing that the service did not admit many long-waiters), and the service continued to breach the incomplete pathways target at month end (showing that they did not find some other solution such as outsourcing or validating their long-waiters).
So, with that fairly strict test in place, here is the data:
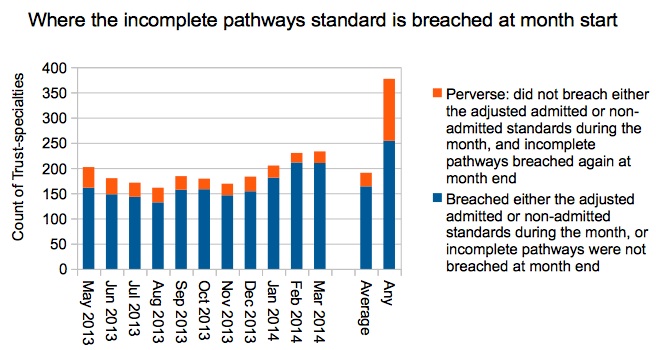
For services that began the month with an incomplete pathways breach, on average 14 per cent of them managed perversely during that month. Over the whole time period May 2013 to March 2014, 33 per cent of those services managed perversely in at least one of the eleven months (and that is shown by the final column labelled “Any:).
Those figures are all at Trust-specialty level, so let’s look to see which Trusts contained specialties that “managed to the target”. That way we can see whether this effect is concentrated in just a few Trusts, or widespread across the NHS. And the answer is that it’s widespread: 58 per cent of Trusts contained at least one specialty that had managed perversely, at an average 1.9 such specialties each.
So we find that the perverse effects of the admitted and non-admitted waiting times targets are widespread and even mainstream among services with 18-weeks pressures. It is encouraging that the other 42 per cent of hospitals were willing to consistently ‘take the hit’ against these targets in order to treat their longest-waiting patients. But the fact that 58 per cent were unable to resist the perverse effects of those targets shows that further change is needed to blunt or eliminate them.
Return to Post Index
Leave a Reply
You must be logged in to post a comment.