Introducing the monthly RTT charts
25/09/2017by Rob Findlay
Your RTT charts are available here
It is all too common for NHS performance reports to say a lot about “what” is happening, but very little about “why”. Sometimes they convey even less information, using red/amber/green ratings to state simply whether a target was met (or not), which at best is uninformative and at worst fosters a blame culture.
So there is a pressing need for performance reporting to be more informative, and to tell a better story about what is really going on. How can we do this for referral-to-treatment (RTT) waiting times?
Many performance measures can helpfully be presented using control charts, which can reveal deeper truths about how performance varies. But unfortunately they don’t work well for RTT waiting times, because they have a cumulative nature, which means we need to take a different approach to understanding the causes of long waits.
So in this piece, I would like to explain the approach we have taken in our monthly RTT reporting, both to help you interpret these reports when you receive them (they are available free of charge here), and to promote the development of more helpful and informative performance reporting across the NHS.
The two causes of long waiting times
Elective waiting times are a function of two things: the size of the waiting list, and the order in which patients are treated. We know this from everyday life: a longer queue means longer waits, and if some people jump the queue then others wait longer.
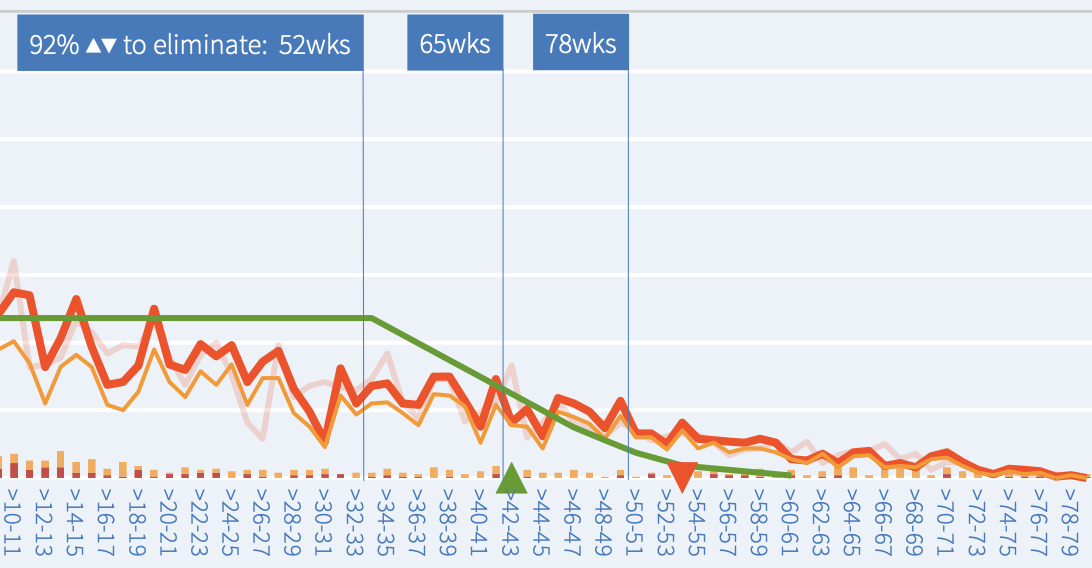
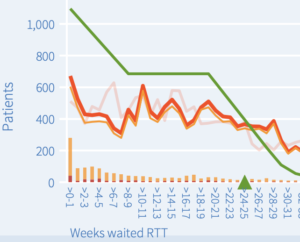
So we need a way of revealing these underlying drivers of long waiting times, and our monthly RTT charts do this by modelling the waiting times that would result from good patient scheduling. Here is an example:
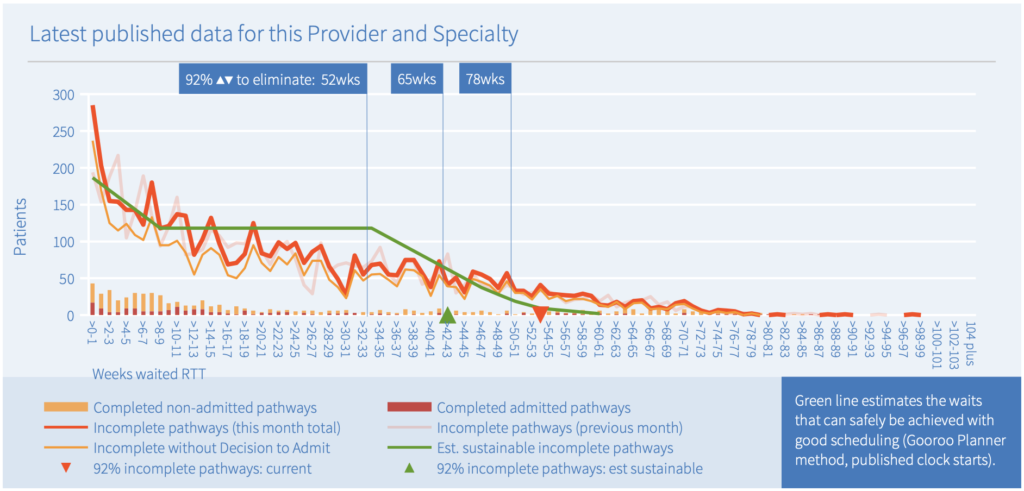
The heavy red line shows a snapshot of the referral-to-treatment (RTT) waiting list (the ‘incomplete pathways’ or ‘PTL’ in RTT jargon) for this service (Ophthalmology at a particular NHS trust). The red triangle shows that 92 per cent of the waiting list extends to nearly 54 weeks. But what is causing this?
If waiting times are too long, then either the waiting list must be too big, or patients must be being treated in the wrong order, or both. We want to know which, and the green line helps us with the answer.
The sustainable waiting time
The green line models the same size of waiting list, but this time on the basis of good patient scheduling. It doesn’t assume a perfect first-come-first-served queue like the one in the Post Office (which is what the commonly-cited ‘clearance times’ would represent), but a more realistic one that takes into account clinical priorities and the disruptions caused by randomness, removals etc.
The formula used is the same as we use in Gooroo Planner, although for these charts we have had to estimate urgency rates from the published data (whereas a local analysis using hospital data would be based on actual patient-level urgency coding).
The green line shows that shorter waiting times should be sustainable in this specialty, and the green triangle shows that waiting times would be reduced to 92 per cent within 43 weeks with good patient scheduling.
It would also be possible to shorten waiting times by reducing the size of the waiting list, which would require extra resources. That would move the green triangle (the sustainable wait) to a shorter waiting time, and if the shape of the list remained the same then we would expect the red triangle (the actual wait) to become shorter too.
The orange line shows how many of the RTT patients do not have a Decision to Admit (DTA) – these patients are the large majority and represent patients who are waiting for outpatient and diagnostic activities. (In some specialties the RTT and without-DTA lines overlap because all treatment takes place in outpatient settings.) Because most of these patients do not yet have a diagnosis, this part of the waiting list is peppered with unknown clinical risks; for some of these patients, the eventual diagnosis will be a clinically urgent condition which has progressed during their wait. So reducing this part of the waiting list is a sensible priority because it reduces the clinical risks as well as reducing the sheer numbers of patients who need to be managed on the waiting list.
Progress towards the ‘eliminate’ targets
In 2022-25 there are RTT targets to eliminate ultra long waiters, so these charts include lines to indicate where the green and red triangles would need to fall below, for those ‘eliminate’ targets to be safely achievable. The ’65wks’ line is drawn at the ’92 per cent within 42 weeks’ position, which allows a suitable margin between the 92nd centile wait and the very longest waiting patient. The calculation method is explained in more detail here.
In our example above, we saw that the actual waiting time is 54 weeks (red triangle), and the estimated sustainable waiting time is 43 weeks (green triangle). The positions of the red triangle relative to the vertical ‘eliminate’ lines show that this service would not be expected to eliminate 78 week waits at the current size and shape of waiting list, although if it improved the shape with better scheduling, pathway management, and resource allocation within the specialty, then the green triangle shows it could eliminate long waiters all the way down to almost 65 weeks. However a reduction in the size of list would be required to eliminate 52 week waits safely.
Waiting times by stage of treatment and subspecialty
What else can the chart above tell us about patient scheduling? Take a look at the columns. They show how long patients had waited when they were treated and discharged (the ‘completed’ waiting times for ‘clock stops’, in RTT jargon). The orange columns show how long the outpatients had waited (‘non-admitted clock stops’) and the red columns show how long the inpatients and daycases had waited (‘admitted clock stops’) at the moment they left the waiting list.
There is a peak in the orange columns at 6-9 weeks, which suggests that new outpatients are commonly seen after a 6-9 week wait which is quite common for a surgical pathway like this. There is also a peak very early on at 0-1 weeks, which probably represents the most urgent elective referrals. Then there are smaller orange columns at higher waiting times, which may represent patients being discharged from clinic following diagnostic scans – these are guesses because unfortunately the published RTT data does not distinguish between these different patients.
The red columns are more spread out, with a peak at around 10-14 weeks. These may represent the typical RTT waiting times for surgery for more urgent patients. The very spread-out nature of the higher clock stop columns might reflect any combination of patients being booked in random order, or different subspecialties having different routine waiting times, or multi-site services having different waiting times on different sites. Unfortunately the published data does not distinguish between these possibilities.
Huge amounts of information
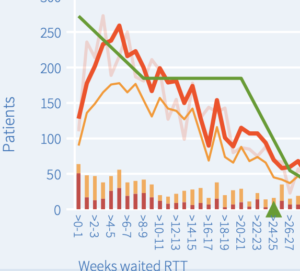
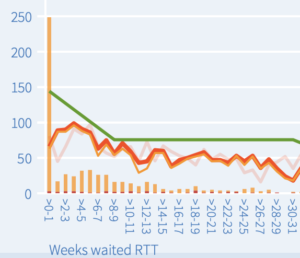
Charts of this kind are capable of revealing huge amounts of information about the service, such as:
- whether long waits are caused by an oversized waiting list, or whether they could be solved with better patient scheduling and internal resource allocation alone (as discussed above);
- whether there is a risk that patient scheduling has reached its safe limits as a tool for achieving waiting time targets (if the sustainable waiting times are longer than actual waiting times);
- whether resources should be shifted between clinic and theatre sessions (if long waits are concentrated in one area or the other);
- whether there are problems with the data quality (although this is sometimes confounded by tertiary referral patterns), for instance:
- delays in recording patients on the system (shown by a dip in short-waiters on the list – see first example below),
- inaccurate clock starts data (shown by the green and red lines approaching the y-axis at different heights – see third example below),
- anomalies where the non-admitted clock stops exceed the supposed clock start rate – see second example below), and
- unexpectedly low or high rates of clinical urgency.
More revealing time trends
Time trends are useful, partly for showing us what has already happened, but also for indicating what is likely to happen next.
The chart below shows the time trend for a range of RTT performance measures.
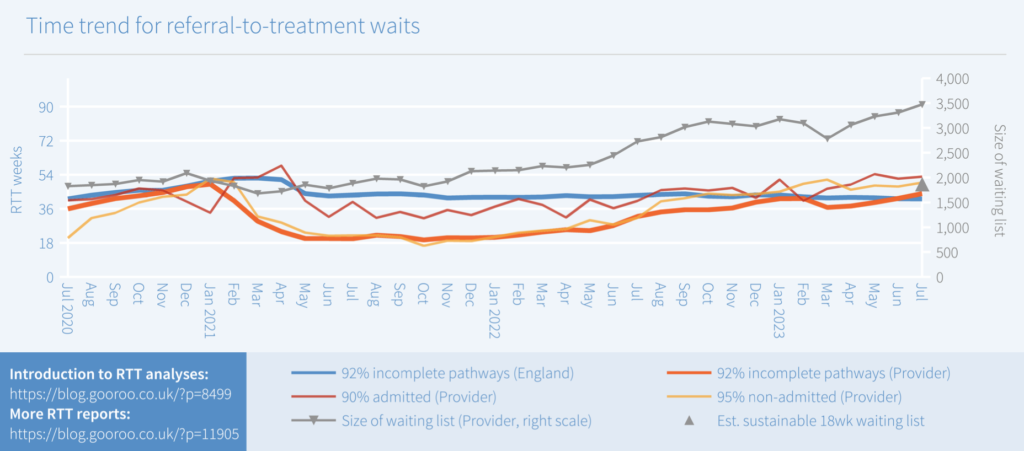
Although the heavy red line attracts the most attention (because it relates to the 18 week target), actually the grey line is the most important one to start with. Put simply, if the waiting list is growing over time then so is your problem – this is the best leading indicator of the pressures to come.
The grey triangle estimates the sustainable waiting list that is consistent with achieving 18 weeks, on the same basis as the green triangle in the first chart above shows the sustainable waiting time. So this chart indicates that the actual waiting list would need to nearly halve in size before the statutory 18 weeks became safely sustainable.
The other lines show the three published 18 weeks measures, and (crucially) they show the position in terms of weeks waited, not as less-informative percentages which fail to show approaching problems as the waiting list grows.
Waiting times are particularly influenced in the short term by patient scheduling. This is typically highly inconsistent in the NHS, as shown in the chart above by the highly variable waiting times for admitted and non-admitted completed pathways.
If there were less variation in those admitted and non-admitted waiting times, that would be a good sign that patients were being scheduled according to their needs, rather than according to the target. It is after all perfectly possible to schedule patients safely and fairly according to their needs, and yet still breach the target because the waiting list is too big.
Limitations of the published statistics
There are limitations to this analysis because of the way the national statistics are collected.
Firstly, these statistics are on an RTT basis so they do not reveal the separate pressures on new and follow-up outpatient waiting times, inpatient and daycase waiting times, and diagnostics.
Secondly, they show the whole specialty in one lump, which is usually alright in some specialties like Urology and Ophthalmology, but less helpful in highly subspecialised ones like General Surgery and Orthopaedics.
Thirdly, the complexities of RTT data recording mean that these statistics are more prone to error and inconsistency than data for each stage of treatment separately.
And finally, they show what just happened, but give only a limited insight into what is likely to happen next.
For all those reasons, you will get more detailed and insightful analyses and forecasts by modelling your local data in Gooroo Planner – if you haven’t seen it recently and would like to, then please get in touch to arrange a free on-site demo.
Return to Post Index
Leave a Reply
You must be logged in to post a comment.